Blood plasma
Blood plasma is the yellow liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular(Within blood vessels) fluid part of extracellular fluid(all body fluid outside of cells). It is mostly water (90% by volume) and contains dissolved proteins, glucose, clotting factors, mineral ions, hormones and carbon dioxide (plasma being the main medium for excretory product transportation). Blood plasma is prepared by spinning a tube of fresh blood containing an anti-coagulant in a centrifuge until the blood cells fall to the bottom of the tube. The blood plasma is then poured or drawn off.[1] Blood plasma has a density of approximately 1025 kg/m3, or 1.025 kg/l.[2]
Blood serum is blood plasma without fibrinogen or the other clotting factors (i.e., whole blood minus both the cells and the clotting factors).[1]
Plasmapheresis is a medical therapy that involves blood plasma extraction, treatment, and reintegration.
Contents |
Fresh frozen plasma and other transfused plasmas
"Fresh frozen plasma" (FFP) is prepared from a single unit of blood or by apheresis, drawn from a single person. It is frozen to −40 °C (−40 °F) after collection and can be stored for ten years from date of collection. The term "FFP" is sometimes used informally to mean any frozen transfusable plasma product, including products which do not meet the standards for FFP. FFP contains all of the coagulation factors and proteins present in the original unit of blood. It is used to treat coagulopathies from warfarin overdose, liver disease, or dilutional coagulopathy. Other transfusable plasma is identical except that the coagulation factors are no longer considered completely viable.[3] This is particularly important for Factor VIII and hemophilia, but these have been mostly replaced by more specific Factor VIII concentrates in the developed world and true FFP is rarely used for that indication.
Plasma used as a source of Cryoprecipitate (Plasma, Cryoprecipitate Reduced) cannot be used for treatment of some coagulation problems but is still acceptable for many uses.
Dried plasma
"Dried plasma" was developed and first used in WWII. Prior to the United States' involvement in the war, liquid plasma and whole blood were used. The "Blood for Britain" program during the early 1940s was quite successful (and popular in the United States) based on Dr. Charles Drew's contribution. A large project was begun in August of the year 1940 to collect blood in New York City hospitals for the export of plasma to Britain. Dr. Drew was appointed medical supervisor of the "Plasma for Britain" project. His notable contribution at this time was to transform the test tube methods of many blood researchers, including himself, into the first successful mass production techniques.
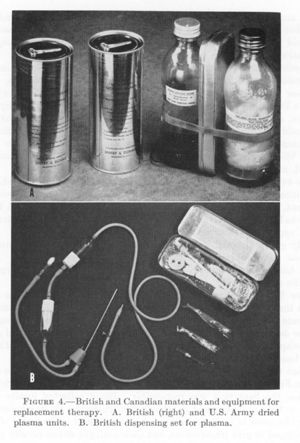
Nonetheless, the decision was made to develop a dried plasma package for the armed forces as it would reduce breakage and make the transportation, packaging, and storage much simpler.[4]
The resulting Army-Navy dried plasma package came in two tin cans containing 400 cc bottles. One bottle contained enough distilled water to completely reconstitute the dried plasma contained within the other bottle. In about three minutes, the plasma would be ready to use and could stay fresh for around four hours.[5]
Following the "Plasma for Britain" invention, Dr. Drew was named director of the Red Cross blood bank and assistant director of the National Research Council, in charge of blood collection for the United States Army and Navy. Dr. Drew argued against the armed forces directive that blood/plasma was to be separated by the race of the donor. Dr. Drew argued that there was no racial difference in human blood and that the policy would lead to needless deaths as soldiers and sailors were required to wait for "same race" blood.[6]
By the end of the war the American Red Cross had provided enough blood for over six million plasma packages. Most of the surplus plasma was returned to the United States for civilian use. Serum albumin replaced dried plasma for combat use during the Korean War.[7]
Composition
|
Reference ranges for blood tests, showing normal mass concentration of blood plasma consituents.
|
|
The same information, shown in molarity rather than mass.
|
Plasma shift
Blood plasma volume may be expanded by or drained to extravascular fluid when there are changes in Starling forces across capillary walls. For example, when blood pressure drops in circulatory shock, Starling forces drive fluid into the blood vessels, causing autotransfusion.
If one stands still for a prolonged period, this causes an increase in transcapillary hydrostatic pressure. As a result, approximately 12% of blood plasma volume crosses into the extravascular compartment. This causes an increase in hematocrit, serum total protein, blood viscosity and, as a result of increased concentration of coagulation factors, it causes orthostatic hypercoagulability.[8]
See also
- Blood plasma fractionation
- Chromatography in blood processing
References
- ↑ 1.0 1.1 Maton, Anthea; Jean Hopkins, Charles William McLaughlin, Susan Johnson, Maryanna Quon Warner, David LaHart, Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1.
- ↑ The Physics Factbook - Density of Blood
- ↑ Blood Plasma Donation Centers Reviewed
- ↑ Transfusion before World War I
- ↑ Plasma Equipment and Packaging, and Transfusion Equipment
- ↑ Hirsch, Eric (1991). What Your 1st Grader Needs to Know: Fundamentals of a Good First-Grade Education. pp 232-233. New York: Doubleday.
- ↑ The Plasma Program
- ↑ Masoud M, Sarig G, Brenner B, Jacob G (June 2008). "Orthostatic hypercoagulability: a novel physiological mechanism to activate the coagulation system". Hypertension 51 (6): 1545–51. doi:10.1161/HYPERTENSIONAHA.108.112003. PMID 18413485.
External links
- Blood plasma pioneer, English physician Gordon R. Ward
- Octapharma Plasma, Inc. - A US-based company which collects human plasma.
|
||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||